|
| Knee and Meniscus AnatomyThe Knee JointMedial Meniscus and Lateral MeniscusThe soft tissue structure in the knee includes 2 menisci, the medial meniscus (located on the inside of the knee) and lateral meniscus (located on the outside of the knee). Menisci are crescent-shaped pads of fibrocartilage that sit on the end of the tibia bone (tibial condyles) and form a concave surface for the rounded ends of the femur bone (femoral condyles) to rest on. They cover approximately 2/3 of the tibia surface (this surface is flat) and are thicker on the outside and thinner on the inside appearing triangular in cross section. The 2 menisci fill the space between the leg bones and cushion the femur so it doesn't slide off or rub against the tibia. 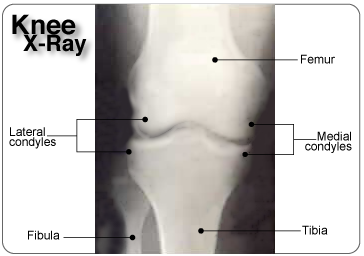 The two menisci are joined together within the knee joint by the transverse ligament. The menisci also attach to leg muscles which help the menisci maintain their position during movement. The semimembranosus and quadriceps attach to both menisci. The lateral meniscus attaches to the popliteus below the knee and the femur via the posterior cruciate ligament (PCL). On the inner part of the knee, the ends of the medial meniscus (known as the anterior and posterior horns) are attached to the tibia and joint capsule and along the exterior edge of the meniscus by the coronary ligaments. This means that the medial meniscus is attached at three points compared to the lateral meniscus which is only attached at two points. Coronary ligaments are loose which allow the menisci to pivot freely. However, because the medial meniscus is anchored by a third point, it does not move as freely in the joint as the lateral meniscus and as a result is torn more frequently. 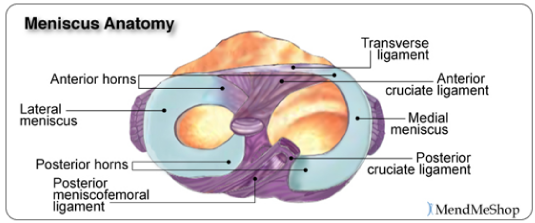 Blood flow to the menisci comes from the inferior genicular artery. The inferior genicular artery artery supplies blood to the perimeniscal plexus which provides oxygen and nutrients to the synovial and capsular tissues around the menisci and within the knee joint. The coronary ligaments attached to the meniscus, transport the blood from the perimeniscal plexus (network of blood vessels) into the peripheral of the menisci. The anterior and posterior horns of the menisci also receive a good amount of blood as they are covered by a vascular synovium. The interior part of the meniscus is avascular, having NO direct blood supply.
The Function of the Meniscus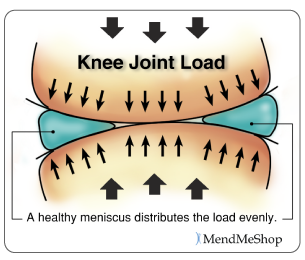 Both the lateral and medial meniscus play a very important role in the proper working of the knee. Essentially, menisci serve as cushions to decrease the stress caused by weight bearing and forces on the knees. They work like shock absorbers, supporting the load by compressing and spreading the weight evenly within the knee. Even while walking, the pressure put on the knee joints can be 2 - 4 times your own body weight; when you run these forces increase up to 6 - 8 times your body weight and are even higher when landing from a jump. By increasing the area of contact inside the joint by nearly 3 times, the menisci reduce the load significantly (dispersing between 30 and 55% of the load). As weight is applied to a meniscus, it becomes compressed and is forced to extend out from between the femur and tibia (squished). However, the circular design of the menisci provides circumference tension (referred to as 'Hoop Stress') to resist this extension and provide stability as the load compresses. If the meniscus is torn at the peripheral (outer) rim, circumference tension is compromised and the meniscus loses its ability to transfer the load and the joint begins to suffer. In fact, if part of the peripheral of a meniscus is removed or a tear extends to the periphery, the load is transferred to the knee joint and may increase by up to 350% causing stress, pain and greater risk of articular cartilage damage. However, if the tear remains on the interior without disrupting the periphery of the meniscus, the meniscus is still able to disperse the load without stress and pain. The menisci also assist with the proper movement (arthrokinematic) of the femur and tibia during flexion and extension. They help stabilize the knees when in motion, reduce friction within the joint, and lubricate and protect the articular cartilage surrounding the tips of the bones from damage due to wear and tear. Your menisci act much like a wedge to help naturally prevent over-rotation in the joint, but just as important, the menisci are the true shock absorbers in the knee joint. When walking, jumping or running, there are heavy forces exerted on the knees; your meniscus absorbs and disperses much of the forces instead of the ends of the bones (where the upper leg and lower leg meet in the knee joint) . If the ends of these bones absorb too much force, they will become damaged. It is also worth knowing that the amount of force exerted on the knee joint grows exponentially as speed of movement increases (ie. from walking to running) 1. If you are already suffering from some meniscus damage, it goes without saying that you want to minimize load on the knee joint when you are upright, so take care to avoid running and/or jumping as load forces multiply quite quickly with faster movements. What is Fibrocartilage?Menisci are composed of tissue called fibrocartilage which is tougher and contains more fiber than other types of cartilage in the body. Fibrocartilage collagen fibers are woven into dense tissue that is resistant to stretching and extending in various directions. This makes fibrocartilage an excellent material for cushioning the knee joint - a joint that is required to move multi-directionally. 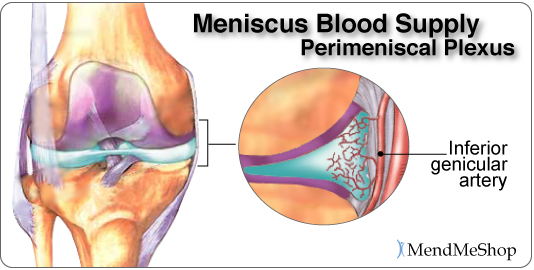 The amount of blood vessels in the fibrocartilage throughout the meniscus varies. The outer one-third of the meniscus is vascular, which means there is an abundance of blood vessels to allow blood to the area. The central part of each meniscus has fewer blood vessels and the inner third does not contain any. As a result, a tear on the outer peripheral of the meniscus can heal faster than one on the inner portion. Tears in the innermost part of the meniscus may not heal completely due to the lack of blood supply. Without proper nutrition (blood supply) the menisci may partially disintegrate resulting in less cushioning and protection within the joint. Proper blood flow ensures nutrients and oxygen reach the area and metabolic waste is removed from the fibrocartilage. When functioning properly, the knee joint naturally receives blood flow through movement and the pumping action of body weight shifting from knee to knee. Greater blood flow results in faster and more complete healing when meniscus or ligament damage occurs. We know the importance of good blood flow into the meniscus, and when your knee is debilitated due to an injury you can see that the lack of movement (and load on the meniscus) will significantly reduce the flow of blood into and around the meniscus. To boost the flow of blood in the knee and maximize the body's healing process - especially when your knee is inactive - you need the proper tools which is why we advocate the use of TShellz Wrap®. Knee Ligaments Ligaments are strong, elastic-like tissues that connect bone to bone and provide stability and protection to your knee joint by limiting forward, backward and sideways movement of the shin bone. The knee has 2 collateral (parallel) ligaments and 2 cruciate (crossing) ligaments. The medial collateral ligament (MCL) and the lateral collateral ligament (LCL) provide support to the knee by limiting the sideways motion of the joint and resisting extreme rotation in a partially flexed position. The anterior and posterior cruciate ligaments (ACL and PCL) stabilize the knee by limiting the rotation and the forward and backward movement of the joint. The MCL is the most commonly injured of the collateral ligaments. Injury is often a result of a blow to the outer side of the knee during sports. Since the MCL is attached to the medial meniscus, damage to the medial meniscus often occurs when the MCL is injured during a hard hit to the knee. The cruciate ligaments (ACL and PCL) are strong and thick providing stability to the joint. Together they work to prevent extreme knee motions of any kind. As a result, any damage to a cruciate ligament can cause noticeable instability in the knee. An ACL injury, the most common cruciate ligament injury, occurs when the knee is locked with the foot planted and the knee is twisted quickly. Athletes required to make sudden directional changes or to slow down quickly as well as those in contact sports are at high risk for ACL tears (soccer, football, tennis, hockey). Minor tears may go unnoticed immediately and will appear a few hours later with pain and swelling. More serious ACL tears are accompanied by severe pain and often a popping sound. With a fully torn ACL, the knee may feel as though something has snapped and walking or bending the knee is usually impossible. The medial collateral ligament (MCL) and anterior cruciate ligament (ACL) are ligaments of interest to meniscus tear sufferers because meniscus tears that occur due to force trauma are sometimes accompanied by tears to the MCL and/or ACL. When the meniscus, MCL and ACL are all injured together, it is referred to as the "unhappy triad". What Happens When the Meniscus is Injured?Menisci tend to get injured during movements that forcefully twist your knee while bearing weight. As we age the meniscal tissue degenerates - getting thinner and becoming weaker overall. A degenerated meniscus, as you can probably infer, is more likely to tear as a result of minor injuries or movements. Regardless of how the meniscus was damaged, once your meniscus is damaged and/or torn, it starts to move abnormally inside the joint. This abnormal movement causes the edge of the torn meniscus to catch between the bones of the joint (femur and tibia). This is usually very noticeable at it can often feel like there is something in there that shouldn't be, or your knee joint won't flex completely, or there is a "catching" and/or "locking" sensation. Your knee then becomes swollen, painful and difficult to move. These injuries can be difficult to heal because blood supply (which helps your body heal itself) is often limited to the outside edge of the menisci. Once you have a meniscus tear, you have an increased risk of developing knee arthritis because these shock absorbers are weakened. They slowly wear away with knee movements and are not able to protect your articular cartilage on the surface of the knee joint as much as before. A point to keep in mind is that if your meniscus is not bearing the load then the load must be born by the articular cartilage - the cartilage that lines the lower end of the femur (thigh bone) and the upper end of the tibia (lower leg bone). The total area where the bones meet is quite small in comparison with the larger impact area of menisci, meaning that the load is spread over a much smaller area of articular cartilage than the meniscus and damage (and loss) of articular cartilage is nearly guaranteed if your meniscus is removed. Physicians and surgeons know the importance of the meniscus and do everything possible not to fully remove a meniscus - they know that it leads to knee osteoarthritis and general loss of function of the knee. Depending of your specific circumstances, your physician may advise a knee joint replacement rather than a full meniscectomy - the function of the meniscus is just that crucial! Do You Really Have Meniscus Injury?Some meniscus injuries are symptomatically similar to injuries listed below. A visit to your doctor can rule out such secondary conditions which is why we also advise getting to a doctor for a proper diagnosis. When dealing with meniscus related injuries, it is not uncommon to suffer from two conditions at the same time. Muscle StrainMuscle strain are commonly known as a 'pulled muscles'. A pulled muscle happens by overstretching muscle tissue beyond its capacity. Athletes are at more of risk of muscle strains as they use their muscles everyday yet less active people also are at risk as their muscles become weak and over using them can strain the tissue. This is why "weekend warrior" type athletes are at high risk of muscle strain - their muscles are not very strong, yet they encounter extreme stresses on the weekends. When a muscle strains, micro-tears happen in the muscle fiber and there may even be separation of the muscle from the tendon. A muscle strain is signalled by pain and inflammation in the muscles - you may feel muscle weakness, swelling, bruising or even pain when move your knee. Ligament SprainSprains happen to ligaments. Ligaments are fibrous tissue that connect bone to bone in the knee joint such as the ACL, PCL, LCL, or MCL. To much force on the joint pulls on the bones and overstretches the ligament tissue, causing micro-tears in ligament fibers. If the sprain is very traumatic the ligament may rupture under the force and surgery will required to reattach the ligament together. Anyone is at risk of a ligament sprain, though some are at higher risk than others due to their activities. An example of activities that are at high risk of knee ligament damage are collision sports such as football or rugby or in sports where there is a lot of direction change while running such as soccer or tennis. Pain and inflammation will arise near the affected ligament; there may also be swelling and pain when move your knee. Bursitis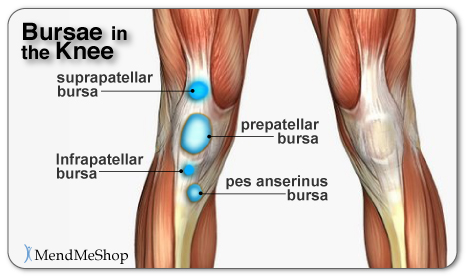 Bursae (plural for bursa) are flattened fluid-filled sacs that function as cushions between your bones and muscles (deep bursae) or bones and tendons (superficial bursae). They reduce friction and allow the surface of your soft tissue to slide over bone effortlessly - without the bursa, the sliding on bone would cause friction and become an irritant. When pressure or friction is too great, excess fluid can build up in the bursa sac causing inflammation; once a bursa becomes inflamed, moving the affected area becomes very painful and movement can be difficult. Any actions that put pressure on the inflamed bursa can increase irritation and cause further inflammation and pain. Arthritis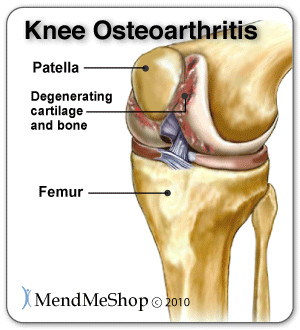 Arthritis is a condition that can affect the tissue lining in joints (this lining is called the 'synovium'). The synovium is a thin membrane that surrounds the entire lining of your knee joint and its main function is to create synovial fluid - a clear fluid that helps nourish and lubricate the joint. Without synovial fluid, friction in the joint increases; this increased friction, in turn, causes more wear and tear on the articular cartilage that line the end of the bones that meet in the knee. Once the articular cartilage is worn through, damage will continue, and penetrate into the bones. You may suffer from rheumatoid arthritis (RA) which is an autoimmune disease, or osteoarthritis (OA) which is a degenerative condition due to wear and tear. As stated elsewhere on this website, the risk of osteoarthritis increases once your meniscus is damaged; if your meniscus is removed, you are almost guaranteed to eventually have osteoarthritis in the knee. When experiencing arthritis in general, inflammation from arthritis causes redness, heat, pain and swelling. Symptoms start with feeling pain and stiffness in the joint, reduced joint mobility, and swelling. It's possible for arthritis to cause tendonitis, with severe swelling in the joint arthritis can cause weakening in tendon tissue resulting in a strain or rupture. Patellofemoral Arthritis causes pain in the front of your knee and can make it difficult to kneel or climb stairs. The kneecap slides up and down in a groove on the end of the thigh bone (trochlear groove). Patellofemoral arthritis occurs when the cartilage along the trochlear groove and on the underside of the patella wears down and becomes inflamed. Cysts in the Knee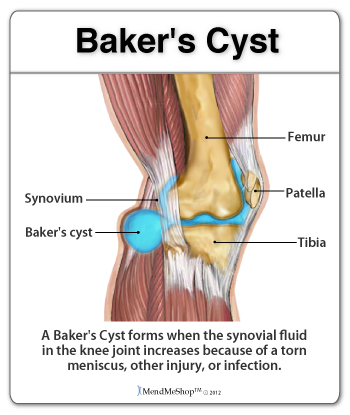 A ganglion cyst or synovial cyst can occur in any joint in the body. A cyst appears under the skin as a lump or bump (non-cancerous) and may sometimes present no other symptoms. The cyst is basically a soft sac filled with a thick, clear fluid. In some cases, the presence of a cyst is due to the breakdown of connective tissue in a joint combined with the accumulation of fluid. A cyst may or may not become painful and in a lot of cases they are harmless; the existence of a cyst may limit your activity and could possibly grow larger if you continue the activity that caused this injury in the first place. Usually cysts only become really painful if the cyst is pressing down on any nerves in the affected area. If this is the case, then you may suffer from pain, tingling, numbness or muscle weakness. Cysts most commonly show up in the wrist, hand, ankle, feet and near other joints (ie. the back of the knee - a baker's cyst). If you don't have a lot of pain then you may only need to treat the symptoms of your cyst and wait for the cyst to naturally go away on its own. It is not uncommon, however, for horizontal meniscus tears to lead to creation of a cyst. In such cases, the cyst is an indication of a more serious meniscal injury, though it is probable that the significant symptoms of a horizontal meniscus tear will not be mistaken as resulting from the cyst. Synovial Plica Syndrome of the Knee (SPS)plicae = plural form of plicaA plica is an inward fold of synovial lining and such plicae are present in most knee joints. Normally, plicae are very thin, flexible and almost transparent. Sometimes the nature of plicae change due to inflammation, and become inelastic, thick and tight; it is in such cases that plicae can cause impingements. A common area of impingement is between the patella the femur (thigh bone) and such impingement would show symptoms of anterior (front) knee pain. Pain usually arise in SPS sufferers when they extend the knee. A cracking noise may also be heard when flexing and straightening your knee. It is theorized that "pathological synovial plica syndrome" is a condition encountered during knee joint formation of the fetus. At the 12th week of life the synovial plica may form in the knee - as we grow and mature this tissue then is becomes entangled within the knee and is unable to dissolve and remains in our adulthood. SPS symptoms are bilateral (meaning it occurs in both knees) in up to 60% of cases, though symptoms do not necessarily show up in both knees at the same time. It is common for this condition to be over looked by doctors. (source: 1.National Library of Medicine) 2.National Library of Medicine) Chondromalacia PatellaCauses a dull, aching pain in the front of your knee. There is damage or softening of the cartilage on the underside of the knee cap. Pain while walking up or down stairs, kneeling or squatting or after sitting for long periods of time with your knee bent. Hoffa's Syndrome / Fat Pad Impingement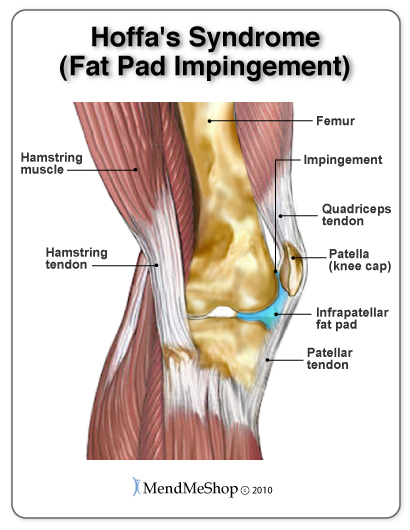 Pain, inflammation, and swelling at the front of the knee cap and along the sides of the patellar tendon. Increased pain when standing for long periods of time, squatting or using stairs and or pain when you extended you knee. Hoffa's syndrome is caused by at pad either suffers a contusion or an injury, resulting in damage and swelling. This can lead to the Hoffa's pad becoming trapped between the femur and the patella every time the leg is extended. Patellofemoral SubluxationPain on the sides and around the knee cap. The kneecap slides up and down in a groove on the end of the thigh bone (trochlear groove). In some people the kneecap is pulled toward the outside of the knee and the kneecap does not slide in its groove. This condition normally affect adolescents and younger children. Mild and moderate cases of meniscus injury are best treated with conservative home therapies. Severe injury to the meniscus will require surgery to bring the edges of the tear together. If you suspect that you've torn your meniscus be sure to speak with your doctor for suggested treatment. Click HERE to Go To Our Online Store We take all major credit cards and Paypal. Product Advisors are available 9:00 am to 5:00 pm Eastern Standard Time Monday to Friday. Learn More About Meniscus Injuries & TreatmentsI want to learn more about Post-Surgery Recovery I want to learn all about Types, Patterns, Shapes & Severity of Meniscus Tears I want to learn more about TShellz Wrap® Circulatory Boost I want to learn more about Ice & Heat: Which Is Better For Treatment? I want to learn more about Meniscus Treatments I want to learn more about different types of Meniscus Surgery
|
        |