|
|
 If all conservative treatment methods have been explored and your symptoms (pain as well as limited use for daily activities) persists, then you will be considered a candidate for surgery. You and your doctor may decide to move forward and have you undergo meniscus surgery, which will trigger the next chapter of your injury recovery journey. Your post surgery rehabilitation efforts will have an important impact on how soon you can return to living and enjoying your normal daily life. The surgery that is selected for your injury will depend on the level of your pain and the amount of damage your doctor suspects there may be to your cartilage and secondary soft tissue (muscles, tendons, ligaments). Much of this damage will be determined through the use of physical exams, x-rays and MRI results. The longer you have waited to have surgery may also be a factor that determines what type of surgery is needed. Muscles begin to atrophy (waste away) only after a few days of disuse. As time passes the muscle fibers shrink and the muscle loses strength and microscopic bits of tissue begin to die inside the muscle. (source: American Academy of Orthopedic Surgeons) If scar tissue is present then a more complicated procedure may be needed to clean out the presence of any scar tissue for optimal healing after the surgery. Your surgeon may make a larger incision into your skin so they're able to fully clean and remove bad tissue . For most soft tissue injuries (including the meniscus), arthroscopic surgery is the preferred procedure as it is minimally invasive and patients usually recover at a much faster rate. This type of surgery will provide the surgeon with first hand insight into the nature of the injury and possibly limit the amount of soft tissue damage from surgery, helping promote a more effective recovery. Some cases however, will require open surgery as the scope of arthroscopic surgery is limited in comparison to full exposure of the knee in open surgery. If you undergo an open surgery you should anticipate a much longer time for rehabilitation efforts. As with any surgery there are risks to every procedure depending on a lot of factors, including your age, the severity of your injury and your level of health going into the procedure. It's always best to discuss all possible risks and complications with your doctor before the procedure. It's important to be aware of the risks you may face with any procedure intended to fix or relieve pain in your knee. Meniscus Surgeries...Joint Arthrocentesis Surgery (fluid drainage)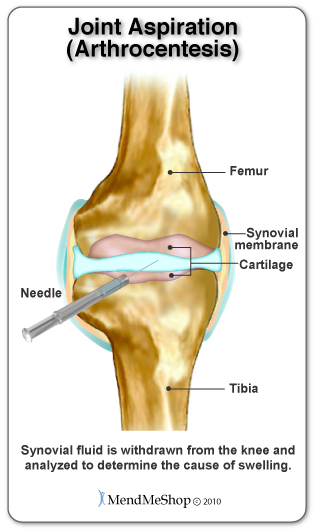 Your doctor will insert a needle into the and drain the fluid. This type of joint aspiration is common when there is fluid in the knee, wrist, hip or shoulder. This type of procedure is used to protect the joint from further (more invasive) surgery and a more complicated outcome. Once you've had your knee drained of the extra fluid, the pressure on surrounding soft tissue (ligaments, tendons, muscle) should be reduced. Even though this procedure may ease your pain, you'll still need to rest the injury and continue with conservative treatment methods for post-surgery recovery. Your doctor will encourage you to use a Cold Compress or Ice Pack at the start to get the swelling down, then eventually progress to stretching/exercise, home treatments such as the TShellz Wrap® and most importantly - rest. Draining extra fluid from your knee isn't a cure for your meniscus injury but it is helpful in dealing with cases where fluid build-up is persistent and painful. This may be used if there is evidence that fluid build-up is problematic in any way, possibly preventing you from day to day activities. Debulking or Debridement This surgical technique is done during open surgery and is undertaken when there is scar tissue, bone spurs, and/or a lot of soft tissue damage in the joint. To perform a debulking or debridement the surgeon will cut away any damaged/inflamed tissue. If muscle or tendon soft tissue is torn or ruptured, they will also scrape down any calcium deposits (bone spurs) that have formed on the bone. Scar tissue may be removed from the muscle fibers, tendons, tendon sheath surrounding the tissue or from both surfaces. Debulking or debridement soft tissue is used as a last resort, if all methods of conservative therapy have been exhausted. Open Knee SurgeryOpen knee surgery is considered to be the "traditional" surgical technique - used when arthroscopic surgery was not yet invented or available. Open surgery is not typically performed nowadays because of the greater tissue trauma due to you having a large surgical incision in your knee - arthroscopic surgery is the preferred choice, when possible. For open knee surgery, the surgeon would open up your knee to view the joint and tissue within, by creating an incision 6 to 10 inches in length. The surgeon must cut through your skin and/or separate muscle, tendons or ligaments underneath, all while avoiding major blood veins and nerves to get a complete visual inside of y5ur 370e. Open knee surgery can take anywhere between 30 minutes to 2 hours depending on the amount of work needed to fix your knee and meniscus damage. During this time you will be placed under general anesthesia to put you to sleep. If there is no open wound in your knee, the surgeon will mark the area they intend to cut into. A tourniquet will be placed just above your knee to prevent swelling and fluid accumulation during the surgery. You will have to stay overnight or perhaps longer in the hospital after your surgery as this allows your surgeon and other doctors and nurses to closely observe your condition after surgery. They will provide stronger medication through your IV to ease your pain and make sure you have no chance of infection or complications after the surgery. Recovery from open knee surgery is much more extensive than recovery from an arthroscopic surgery. Notable complications, such as blood clotting and infection, are higher risk factors during an open knee surgery versus an arthroscopic procedure. As with any surgery, it is important to discuss all possible complications with your orthopaedic surgeon before the procedure. Arthroscopic Meniscus Knee SurgeryThe size and location of the tear as well as activity level are taken into account when determining if arthroscopic surgery is right for you. An arthroscopic procedure is done with 2 to 4 small keyhole incisions approximately 4 to 5 mm in length, a thin tube containing a camera and light inserted through an incision near the knee joint. This type of surgery will provide the surgeon with first hand look into the nature of the injury and possibly limit the amount of knee damage from surgery, helping promote a more effective recovery. Some tears however, will require open knee surgery as the scope of arthroscopic surgery is limited in comparison to full exposure of the meniscus in open surgery. 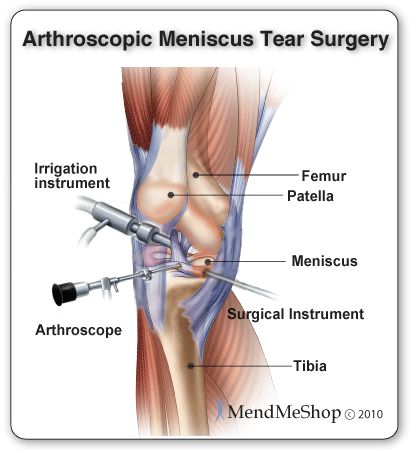 You will also be prepared for surgery with local, regional or general anesthesia. Local anesthesia focuses on numbing your knee; regional anesthesia numbs you below the waist while general anesthesia puts you to sleep. During arthroscopic surgery, a tourniquet will be placed above your knee to prevent swelling and fluid build-up. Surgical instruments are then inserted through these incisions. Your surgeon will insert the instruments required which may include probes, scissors, shavers or lasers. In order to view your inner knee joint and have enough room to move around, your surgeon will inject a saline solution into your knee. The knee will expand space is created between your femur and tibia. If your meniscus tear is a similar shape, size and in a location that your surgeon already expected and you qualify for a meniscal repair (versus removal), then a repair of the meniscus will be performed. The surgeon will take 1 to 2 hours to complete arthroscopic meniscus repair surgery. An arthroscopic meniscal repair is generally considered to be an outpatient procedure, so most of the time you will be able to leave the hospital the same day as your surgery. 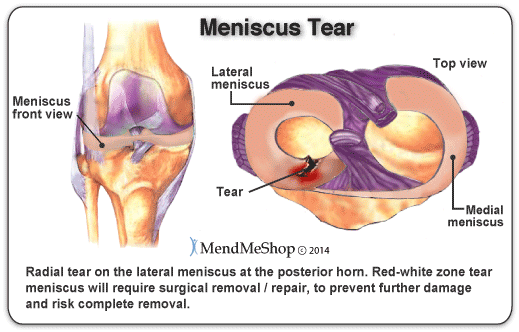 Only about 10 - 15% of meniscus tears are repairable, and in most of those cases the meniscus is repaired along with other tissue in the knee (MCL or ACL). If your orthopedic surgeon has decided that you qualify for a meniscal repair procedure, your surgeon may fix your meniscus with one of the 3 techniques available to fix a meniscus tear:
Before your surgeon uses one of these techniques to fix your meniscus tear, they will perform additional work called debridement and abrasion to prepare your tissue for the repair. Debridement of your meniscus tear is done in order to remove dead, hardened, or contaminated tissue. If you have an open wound the removal of any foreign substances found in the knee will be done. Your surgeon will then scrape down and smooth out (abrade) your tissue to make it easier for the edges of your tear to come together. Abrasion can also trigger bleeding of your meniscal tissue. Bleeding in your meniscus is something that your surgeon wants to happen because it will stimulate healing of your meniscus after the surgery. The technique selected for your surgery can greatly influence the healing response of your meniscus to the surgery. The right technique for your tear can increase your meniscal stability and speed your overall recovery.
Meniscus Repair for a Torn MeniscusA meniscal repair is generally preferred over a meniscectomy, as it fixes the damage and helps prevent total breakdown of your meniscus. However, this involves a more complex surgery, the recovery is longer and it is not always possible (depending on the location). Early diagnosis affects the outcome of this surgery. Younger people tend to be the best candidates as their tears are often stable and located near the outer blood rich area of the meniscus. These tears have a better chance of healing than those farther in the joint because of the blood supply  Trepanation (Abrasion Technique) involves making small holes or shaving torn edges in your meniscus to promote bleeding and enhance healing. Longitudinal tears or bucket handle tears often won't heal unless they are abraded. Suturing involves using stitches to reconnect the tear, repair the damage, and save your meniscus. The sutures are spaced 3-4 mm apart to prevent gapping and sewn while your knee is fully extended (or at 10 degrees maximum) to allow for full extension after surgery. Arthroscopic Partial Meniscectomy Surgery & Arthroscopic Full Meniscectomy SurgeryPartial Meniscectomy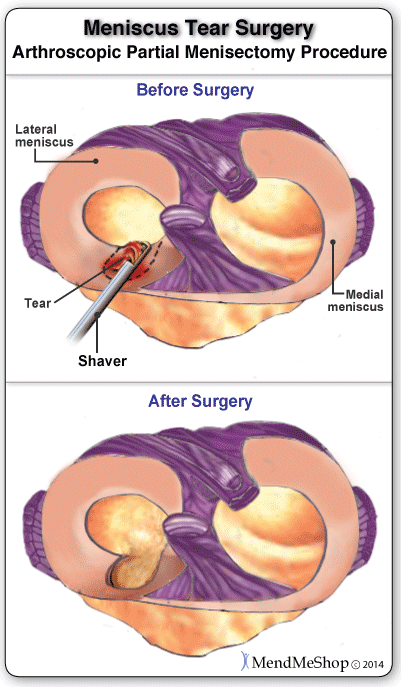 The most common meniscus surgery is a Partial Meniscectomy or Resection, which involves removal of the torn or damaged part of your meniscus. Partial removal of the meniscus will depend on the tear factors; location, the way it is torn, the length, condition of the entire knee, condition of the entire meniscus, your age and any related degeneration (such as arthritis). It is generally used for degenerative and horizontal tears located in the inner 2/3 of your meniscus (the white-on-white zone). This area has a poor healing rate because it receives little or no blood supply, therefore it is better to remove the damaged part rather than try to fix it . The goal of this surgery is stabilization, which will prevent catching, buckling and locking in your knee joint. The surgeon will trim and smooth out frayed edges on the inner rim (which can be difficult to reach), and remove the damaged part or flap of your meniscus. You should be aware that long term degeneration of the knee is more likely the more meniscus tissue is removed, and your surgeon will try to save as much of the meniscus as he/she as possible. Full MeniscectomyFull meniscectomy may be required if there is extensive damage to the meniscus and it is determined unsalvageable. Removal of the meniscus can lead to joint narrowing, ridging, flattening, and becoming bow-legged or knock-kneed. Once the meniscus is removed there is much less cushioning in your knee and as less stability (resulting in a 200%-350% increase in contact pressure). A full meniscectomy is more common in elderly people than the young and active, as the impact of a fully meniscectomy will last for lifetime and can be a big impact on one with an active lifestyle. Studies have shown that over 75% of patients that have undergone a partial meniscectomy have been able to go back to doing what they did before their meniscus injury. Although meniscectomies have faster recovery than other meniscus surgeries they can often lead to arthritis as the size of your meniscus (shock absorber) is reduced and/or removed. Normal knees have 20% better shock-absorbing capacity than meniscectomized knees. An arthroscopic partial meniscectomy will usually take 1 to 2 hours to complete. It is also an outpatient procedure, so you should be able to leave the hospital the same day as your surgery. Post-surgical recovery of a partial meniscectomy is much quicker than rehabilitation for a meniscal repair. Once your torn meniscus tissue is removed your symptoms should ease and you will be able to return to your regular activities (work or athletics) within 1 to 2 months. Arthroscopic Meniscal Replacement Surgery In early medical practices the menisci were thought to be pieces of tissue that had no function in the knee. This school of thought, many doctors and surgeons would regularly remove an entire meniscus in order to treat the pain from the symptoms their patient experienced. Medical practices do evolve over time, and now so much more is known about the function of our menisci and how important they truly are. Now it is also obvious why those who have previously had a full meniscectomy are experiencing so many long-term chronic symptoms. Meniscus removal may have bone spurs that have developed around their femur as well as a narrowed joint capsule and a degenerative condition such as arthritis or osteoarthritis (OA). This procedure is still considered to be experimental in nature and there are few people who qualify for this surgery. In order to qualify you must meet the following criteria:
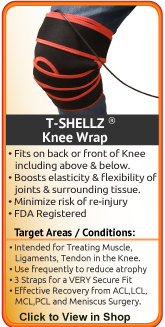
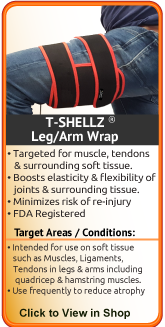
If you do not meet this set of criteria, your doctor or surgeon may feel that there are too many chances for a negative outcome and so they will not perform this surgery. Your surgeon will only consider this procedure if they think you will experience the best possible results from this surgery. A meniscal replacement involves implanting a new meniscus into your knee. There are two different replacements that can be used: AllograftAn allograft is a transplant from a donor. A good candidate for this type of replacement is someone who is young, has minimal ACL damage, is a previous meniscectomy patient, and has developed pain in the knee capsule. If you are obese, suffer from gout or arthritis, have an infection or any metabolic disease (being unable to convert food to energy) then you are not a likely candidates for this procedure. The success of this surgery is dependent on proper knee alignment, ligament stability, and amount of articular cartilage that is present. Collagen ImplantA collagen implant is also an option to replace the meniscus. The implant is stitched into place with the hope that your body begin to grow new meniscal tissue by attaching itself to the porous surface of the implant. In this way, the implant works as a scaffold to assist the body with its own repair process. Some negatives are often experienced with meniscal replacements - such as a build of scar tissue inside the knee. This scar tissue buildup prevents full range of motion and can lead to osteoarthritis in the knee. (source: U.S. National Library of Medicine) Further to this, the failure rate of synthetic meniscal implants are significant. (source: boneandjoint.org.uk) Stability of your Knee Joint after Meniscus SurgeryIt is important to understand that surgery may not give you back 100% functionality of your knee joint, but you should be able to return to most if not all of your pre-injury activities. Surgical procedures (outlined above) are often performed with very successful results. What will truly make a difference in surgery recovery is your commitment to a doctor recommended rehabilitation program. After surgery there is always a possibility of re-injury even after a surgical procedure and it becomes extremely important to carefully follow and adhere to the rehabilitation program while taking adequate rest as advised. One complication of surgical repair for muscle/tendon tear is that skin can become thin at site of incision, and may have limited blood flow. The load distribution across the knee will be directly related to the amount of meniscus that is removed during surgery. With less meniscus tissue between the upper and lower leg bones, the joint will be less able to handle heavier loads. The uneven load distribution caused from the reduction in meniscus tissue, may increase knee degeneration in the joint. Lack of knee stability is often accompanied with pain while walking, running and jumping and may require you to wear a brace or use crutches. Overall, the knee is less likely to be as active as it once was and this will increase your risk of knee joint degeneration. By implementing a proactive conservative treatment protocol that involves the use of a Cold Compress or Ice Pack to keep inflammation and swelling down, the Knee TShellz Wrap® to combat range of motion loss and promote more blood flow in the area, and consistent use of Passive Knee Stretches you can help lessen the chance and/or severity of knee joint degeneration and in some cases, our customers have prevented the onset of degeneration through regular use of these treatments. In the case of a discoid meniscus that did not heal through conservative treatments, part of your meniscus may be removed to relieve symptoms, prevent further tearing and preserve some of your meniscus cushioning function. Ask any doctor and they will tell you that the success of your surgery depends on your level of dedication to your recovery. Many of our meniscus surgery post-op clients have achieved great success through regular use of conservative treatment protocols, including the use of a Cold Compress or Ice Pack and a Knee TShellz Wrap®. Using these physician approved conservative treatment therapies will lessen the risk of re-injury, degeneration and muscular atrophy during your rehabilitation process. Many of our successful clients have combined these therapeutic treatments with a rehabilitation plan recommended by their doctor, surgeon or physical therapist. Surgery RehabilitationClick here to read about meniscus post-surgery rehabilitation. Product Advisors are available 9:00 am to 5:00 pm Eastern Standard Time Monday to Friday. Learn More About Meniscus Injuries & TreatmentsI want to learn more about Post-Surgery Recovery I want to learn all about Types, Patterns, Shapes & Severity of Meniscus Tears I want to learn more about TShellz Wrap® Circulatory Boost I want to learn more about Ice & Heat: Which Is Better For Treatment? I want to learn more about Meniscus Treatments I want to learn more about different types of Meniscus Surgery
|
        |